Fourteen years after making a landmark discovery, a team of Toronto researchers has received Health Canada approval to test a homegrown innovation in a world-first clinical trial.
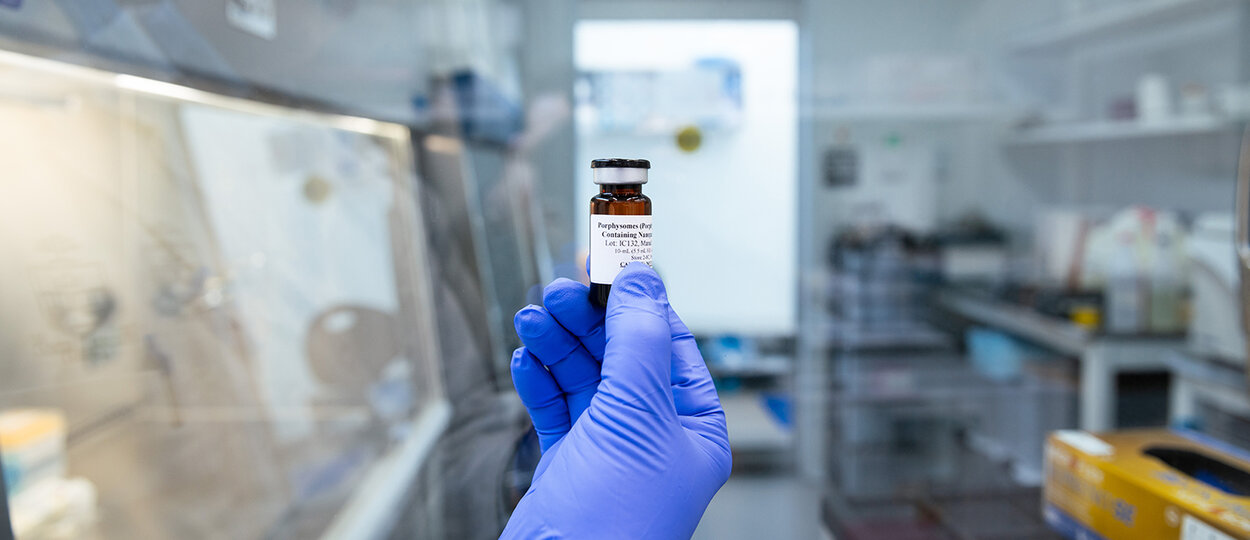
The trial will test for the first time in humans a new type of nanoparticles called porphysomes, which have the potential to improve how we detect and diagnose cancers and make treatments less invasive.
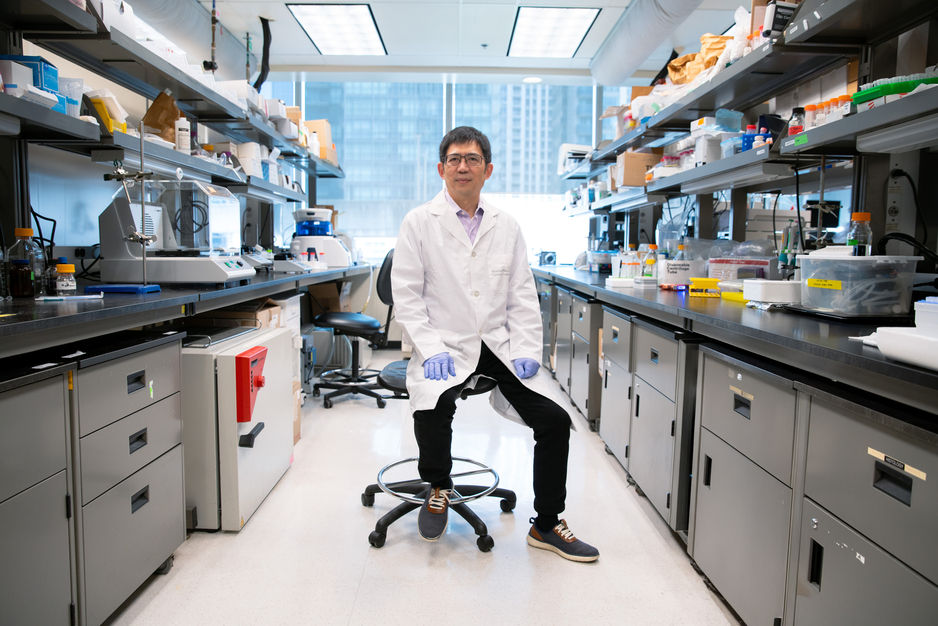
“Porphysomes are a first-in-class lipid nanoparticle to have intrinsic multifunctionality covering multiple cancer types and different clinical applications,” says Gang Zheng, associate research director of the Princess Margaret Cancer Centre, University Health Network, professor of medical biophysics at U of T’s Temerty Faculty of Medicine, and professor - status at the Leslie Dan Faculty of Pharmacy.
Zheng’s team created porphysomes in 2011 after failed attempts to load large amounts of porphyrin, an algae-derived pigment with therapeutic potential, into conventional lipid nanoparticles. Led by graduate student Michael Valic, the researchers spent the next decade embarking on a journey to translate this serendipitous discovery from bench to bedside.
They described key traits about porphysomes including their ability to naturally accumulate in tumours but not in healthy tissues, and to absorb light for both imaging and light-based therapies that target cancer cells. The new nanoparticles could also be used to deliver drugs to tumours and to bind radioisotopes for PET imaging or radiotherapy.
Remarkably, the researchers saw the same exciting results in multiple different cancer types — including colon, lung, oral, ovarian, pancreatic and prostate — and across a wide span of preclinical models.
In the next stage of this work, Zheng and a team of clinical researchers at UHN are set to launch a first-of-its-kind clinical trial to assess the safety of porphysomes in 15 patients with advanced ovarian cancer. The trial team is co-led by Stéphanie Lheureux, a clinician investigator at UHN’s Princess Margaret Cancer Centre and an associate professor of medicine at Temerty Medicine, and Amit Oza, head of the division of medical oncology and hematology at Princess Margaret and a professor of medicine at U of T.
Because the porphysomes will be labelled with a radioactive form of copper called copper-64 (Cu-64), the researchers can also track where the nanoparticles go and how quickly they break down.
The phase 1A trial is a big step forward in bringing this made-in-Toronto innovation out of the lab and into the clinic, but getting here wasn’t easy.
One of the biggest hurdles the research team faced was proving to Health Canada that they could produce clinical grade Cu-64-labelled porphysomes that met the quality standards for human drugs.
To address this challenge, Zheng enlisted the help of Raymond Reilly, a professor in the Leslie Dan Faculty of Pharmacy and the director of the Centre for Pharmaceutical Oncology. As a trained nuclear pharmacist, Reilly’s expertise in making clinical quality radiopharmaceuticals — drugs that contain a radioactive isotope — was instrumental in helping the researchers scale up from preclinical to clinical studies.
Reilly also oversees the CPO’s Good Manufacturing Practices (GMP) facility, a production site where radiopharmaceuticals are made to strict quality standards for human use.
“This facility has allowed us to support a lot of different collaborative and translational research opportunities because we provide the necessary bridge step to move from preclinical to human studies,” says Reilly.
To secure Health Canada approval for the porphysome trial, Reilly and his team made several batches of Cu-64-labelled porphysomes that passed multiple quality assurance tests. He notes that because of the short half-life of Cu-64, each dose of the drug must be custom made when a patient is enrolled. The radioactive copper is made and shipped from the University of Wisconsin–Madison to the GMP facility at the CPO, where it is attached to porphysomes. Reilly’s team tests each batch before it is delivered via a special courier to the clinical trial team at Princess Margaret.
“Professor Reilly’s part in developing the GMP protocol for the Cu-64 radiolabelling of porphysomes was critical in Health Canada’s decision to approve our clinical trial,” says Zheng.
“Without Professor Reilly and the GMP facility, the journey to bring this discovery to patients would have been even longer.”
“Without Professor Reilly and the GMP facility, the journey to bring this discovery to patients would have been even longer.”
Positive results from this trial, which Zheng hopes will be complete within the next year, would pave the way for a phase 1B trial to assess the safety of porphysomes in patients with different cancer types.
“I believe the biggest potential for porphysomes is in minimally invasive treatments for early-stage cancers like early-stage lung cancer,” says Zheng.
Back in the lab, he and his team are working to understand why porphysomes accumulate in tumours and how they generate an immune response beyond the cancer site.
For Reilly, the successful launch of this clinical trial is a testament to the power of collaboration in taking innovations from the lab into the clinic.
“Porphysomes are a homegrown technology discovered here in Toronto and it needed a homegrown solution to take it to the next stage. It was the perfect opportunity to link the expertise and resources we have at U of T to advance a new cancer nanomedicine that could potentially impact patients around the world.”
This work was funded by the Ontario Institute for Cancer Research, Princess Margaret Cancer Foundation and Terry Fox Foundation. The GMP facility was supported by funding from the Canada Foundation for Innovation and Ontario Research Fund and by funds from the Leslie Dan Faculty of Pharmacy.
More News
Image
Grad to Watch: Jackie Fule Liu’s research focuses on better outcomes for diabetes patients
A recent PhD graduate, Jackie Fule Liu combines hands-on skill and big-picture thinking to help tackle diabetes care challenges.
Read More
Image

U of T community members recognized with Order of Canada
Congratulations to Dean Emeritus and Professor K. Wayne Hindmarsh on his appointment.
Read More
Image

Welcoming Ivy Lam as Academic Lead in Climate, Health & Sustainable Care
Assistant Professor Lam will guide the Leslie Dan Faculty of Pharmacy's efforts to embed environmental sustainability across the Faculty.
Read More